Every month I try to read an open-access article. After reading the article, I share the title and associated link with my followers. This is to encourage clinicians to read articles, stay up to date, and continue to grow.
This article is about COPD and COPD exacerbation. The authors describe the objectives of this paper as following:
The first objective of this study was to evaluate whether the data from the ECLIPSE and SPIROMICS studies support the presence of an individual-specific, underlying AECOPD rate which is stable over time. The second objective was to explore, based on the findings from the first objective, the randomness of observed AECOPD counts in a 12-month period, in order to determine the suitability of this factor for phenotypic classification.
p2
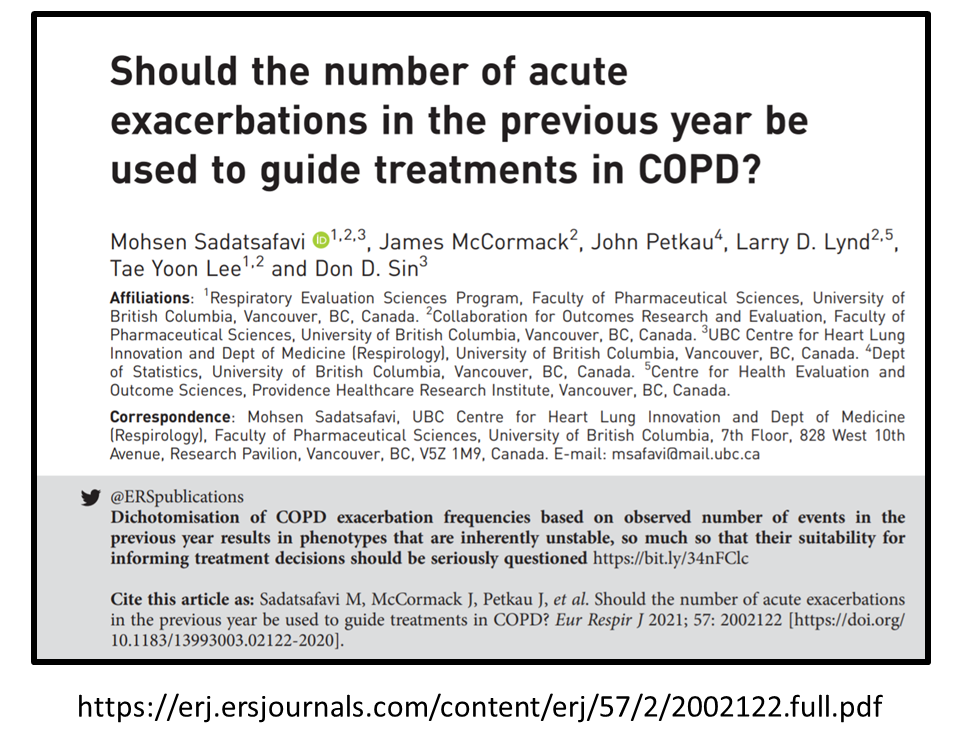
Should the number of acute exacerbations in the previous year be used to guide treatments in COPD?
By: Mohsen Sadatsafavi, James McCormack, John Petkau, Larry D. Lynd, Tae Yoon Lee, Don D. Sin
European Respiratory Journal (ERJ) 2021 57: 2002122; DOI: 10.1183/13993003.02122-2020
Link to the journal ERJ: https://erj.ersjournals.com/content/57/2/2002122?etoc
Direct link to the article (pdf): https://erj.ersjournals.com/content/erj/57/2/2002122.full.pdf
Reasons I enjoyed reading this article
- It makes you appreciate the complexity involved in predicting future COPD exacerbation. It is not as simple as looking at a patient’s number of exacerbations in the previous year.
- The ECLIPSE and SPIROMICS studies are looked at and comments are made about the “difference” in findings.
- It is always nice to see the work of Canadian clinicians and researchers!
Read the article and let me know what you think! What are the factors used by your organization to predict and prevent future COPD exacerbations?
Happy learning and reading!
Farzad Refahi
March 28, 20201
https://respiratory.blog/lets-read-an-article-a-month-march-2021/