Every month I try to read an open-access article. After reading the article, I share the tittle and associated link with my followers. This is to encourage clinicians to read articles, stay up to date, and continue to grow.
Link to the article: https://erj.ersjournals.com/content/56/6/2000556?etoc
Link to the blog post: https://respiratory.blog/lets-read-an-article-a-month-february-2021/
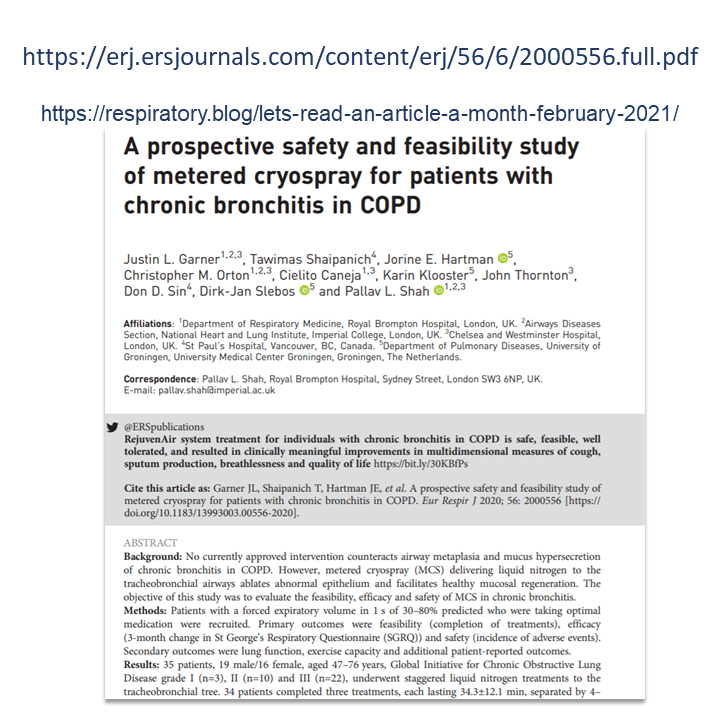
This month I found a great piece to share with you. This one is a prospective, open-label, single-arm study. The objective of this paper is to “evaluate the feasibility, efficacy and safety of metered cryospray therapy to treat patients with chronic bronchitis in COPD” p3.
A prospective safety and feasibility study of metered cryospray for patients with chronic bronchitis in COPD
By Justin L. Garner, Tawimas Shaipanich, Jorine E. Hartman, Christopher M. Orton, Cielito Caneja, Karin Klooster, John Thornton, Don D. Sin, Dirk-Jan Slebos and Pallav L. Shah.
Eur Respir J 2020 56:2000556; published ahead of print 2020,
doi:10.1183/13993003.00556-2020
Link to the article: https://erj.ersjournals.com/content/56/6/2000556?etoc
Reasons I found this article interesting
- I didn’t know about metered cryospray therapy (MCS) and this article introduced me to its application in chronic bronchitis. Its intent is to “cryoablate abnormal epithelium and excessive mucous-producing goblet cells” p2.
- The method of application is clearly explained in this article. On page 3, the authors explain the three treatments and which lobes and airway pathways received the MCS therapy in each of those treatment sessions.
While I am still unsure about the safety of this therapy until further research and improvements are done, I enjoyed learning about the unique approach. I say this as the sample was only 34 subjects. Also, “no definitive histological differences were observed between baseline and day 60 endobronchial biopsies” p10.
If you were not aware of this therapy, this may be a good article for you to read. If you have applied this therapy in the past, I would love to hear about your thoughts and experiences. Leave a comment and let me know!
Happy learning!
Farzad Refahi
Feb. 1st, 2021
https://respiratory.blog/lets-read-an-article-a-month-february-2021/