What do my respiratory therapy blog and Innisfil Brazilian Jiujitsu have to do with each other? Do I practice Jiu-jitsu?
The fact that I had to look up the spelling of this sport should give you a clue. I am sure it is a great sport and can help people destress. I yet to try it, but hopefully one day. This blog post is a reflection than an informative respiratory therapy piece.
With the start of the pandemic, I was deployed to the acute care side of respiratory care. I had to push through personal and mental barriers, step out of the comfort zone, and help out where my presence was required. While uncomfortable, I was fortunate to have a job. I was lucky to rely on a steady paycheque. Not everyone has had the peace of mind when it comes to income. Many small businesses have suffered. To answer the question I asked at the beginning of this blog post, the common denominator of my blog and IBJJ is people. This is NOT a paid promotion. I have purchased a few of my friend’s merchandise and now I am shamelessly promoting his business. My friend PK opened his business in 2019 ( 1035 Cole Street. Innisfil, Ontario). I am looking forward to the day that he re-opens his gym, and does what he enjoys.
Since the start of the pandemic, I have seen many acts of kindness. Many people donated masks and food to hospitals. Something I benefited and very thankful for. I have also observed front line workers giving back.
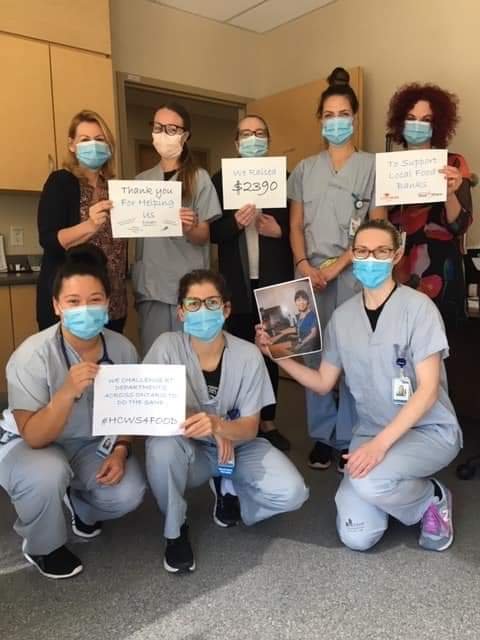
Respiratory Therapy Society of Ontario (RTSO) recently shared these photos of RTs and organizations on social media (July 6th, 2020):
RTs and other healthcare workers joined to raise money and give back to their communities. #HCWS4FOOD.
Take a step back and evaluate your situation. Is there any way you can give back? Any way you can help out someone in need? Our experience has been different and we may be in different stages and financial situations so this is not put to push pressure on anyone. Giving back could even be volunteering and offering your knowledge and skills. If you don’t have the time or the money to give back, take a moment and appreciate what and who you do have (give gratitude).
#StrongerTogether
This is also a perfect opportunity for me to thank John Meloche from Melotel Inc. for offering his expertise and services to me so I could offer my respiratory therapy blog to those who could benefit from it!
Farzad Refahi
July 8th, 2020
https://respiratory.blog/Brazilian-Jiujitsu/