Thank you Rebecca for bringing home the gold medal and the shout-out to all hardworking RTs out there!
It has been a hard two years but we can do it!
#strongertogether
Respiratory Therapy by Farzad Refahi
With a goal of improving the life of healthcare providers as individuals and as clinicians.
Thank you Rebecca for bringing home the gold medal and the shout-out to all hardworking RTs out there!
It has been a hard two years but we can do it!
#strongertogether
Here is a hello, bonjour and shout out from the iconic voice of Toronto Raptors’ Jack Armstrong! Dedicated to all the amazing RTs!
Music: Feeling Fine
Musician: Uncleboris
URL: https://icons8.com/music/
Purchased content from Cameo
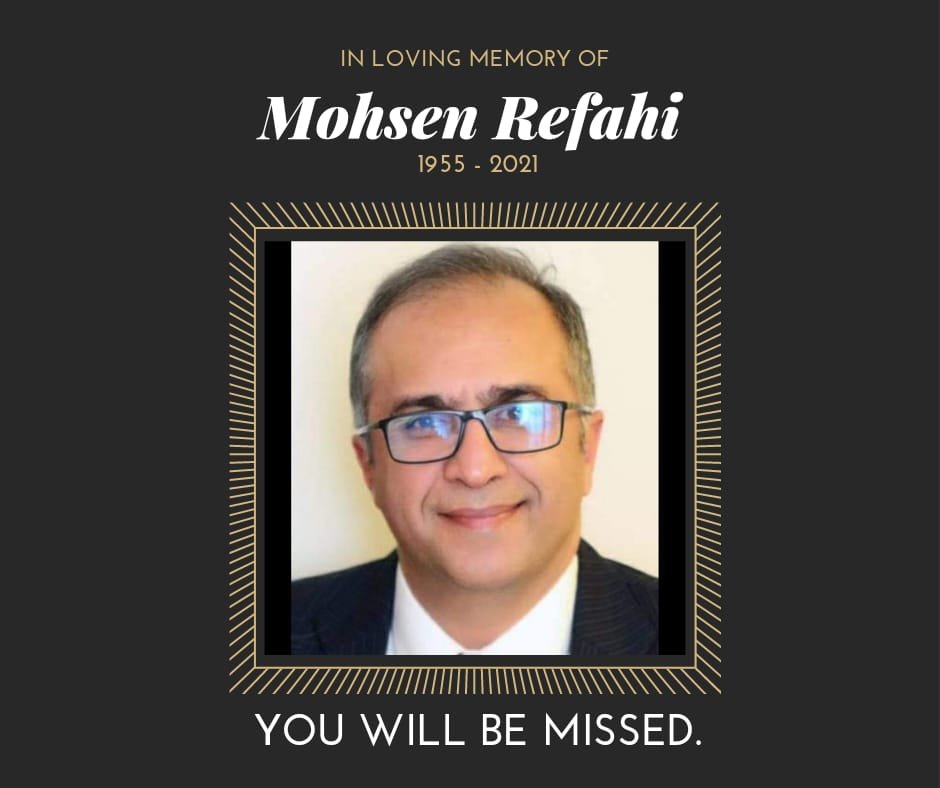
This post is dedicated to my father. He was a kind hearted man who worked hard to have a humble and good life for the family. My father and mother have been a great role models for my brother and I. While he was taken away way too sudden and soon, I am blessed to have had him in my life.
Thanks for all you have done for me, dad.
With love,
Farzad
Thank You – RT Week 2020
It is my tradition during RT Week to sit back, reflect, and thank those who have made a positive impact on my respiratory therapy career over the past year.
As I finish my third and final year as a Director with the Respiratory Therapy Society of Ontario (RTSO), Nancy Garvey’s name comes to mind. Nancy recruited and mentored me three years ago and I am very grateful to her. I have witnessed the amazing work of many individuals who not only prevented further financial turmoil but brought stability and growth for the organization. This stability helped the organization to provide resources and advocacy for RTs during the 2019-2020 pandemic. There are many great people within the organization so it is hard to name just a few for this post: Gino DePinto, Sue Martin, Kelly Hassall, Shawna MacDonald, Sue Jones and Susan Aikenhead. It has also been nice to begin working with Megan McFarlane, Paula Smith, Greg Donde and Wendy Foote! Tony Kajnar is also part of the team, and also continues to contribute to our profession in various organizations!
I had a unique opportunity to join a team of panelists in the creation of a joint statement by CTS and CSRT. Thank you, Carlyn McCoy, Micah Cooperberg and Elizabeth French for this opportunity! https://www.csrt.com/wp-content/uploads/CTS_CSRT_COVID_PFT_Final-July12_2020.pdf
Many RTs volunteered to share their insights and experiences with me over the years and I am very grateful to them! Over the last 12 months, I spoke with Rachel Nesbitt, Kelly Hassall and Dave Wall.
Thomas Piraino dedicated his evenings for a period of time to RTs, assisting with their questions during the pandemic. I am thankful for the sense of reassurance he brought to me and the RT community.
As always, a big thank you to my lovely wife, Jessica, who continues to support me in this journey.
I began this blog to help RTs, and I wouldn’t be here without the help and support of my amazing followers. Much appreciation and love to you all!
Happy RTing!
Farzad Refahi
Oct. 25th 2020
https://respiratory.blog/RTWeek2020/
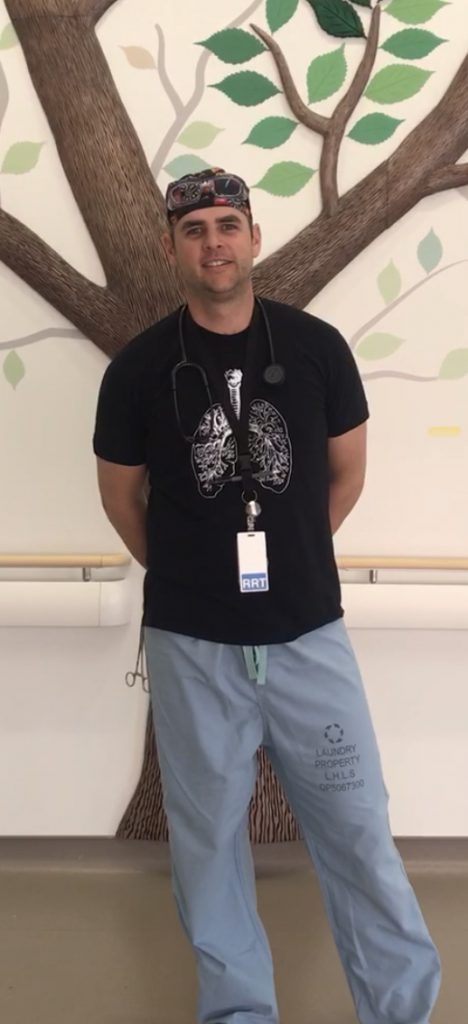
Are you interested to hear insights from someone who is an RRT, an AA, an instructor and volunteer? Then you will greatly enjoy my conversation with Mr. David Wall. I met Dave through Gino De Pinto at a CSRT conference. I also had the opportunity to watch Dave’s great presentation at the same conference. Dave and Greg Donde are the hosts of RT Audio podcast. I reached out to Greg to ask him about Dave.
Dave is a great classmate, friend, co-worker, and mentor. We graduated together from Fanshawe’s Respiratory Therapy Program in 2006; have worked together in various clinical settings over the years and now teach together. We often throw ideas off each other and have a long list of ambitions we would like to work on over the next few years to improve the program. Some of these are realistic ideas and others are pipe dreams. Either way, he is always thinking “what’s next”. I always appreciate the critical feedback that Dave provides when I ask him “can you have a look at this”. He has an innate ability to break down complex concepts and loves to gamify teaching. Students always love the annual Sputum Cup which challenges their knowledge, skills, and ability to work together.
Greg Donde. October 2020
Thank you, Greg! I am not going to keep you all waiting any longer. Please enjoy my conversation with Dave!
I was in my 3rd year of studies at the University of Guelph where I was completing a physical chemistry course and somewhat frustrated with what I was learning and envisioning how to apply this to my life. In fact looking back I was just confused on where my life was headed while studying a subject that I enjoyed but one that I wasn’t sure I wanted to do for the rest of my life. I remember calling my sister who was at the time a Nuclear Medicine Tech in Toronto and I guess I was complaining a bit too much when she abruptly stopped me and said “why don’t you come see me this weekend”. I took her up on the offer and spent the weekend with her and her room-mates, one of which was an RRT working at Toronto area hospital. Her room mate was talking about her previous shift and I was immediately intrigued. I started to look into the profession and felt that everything I was learning was something that I would enjoy. I finished my degree at Guelph and the following September was enrolled at Fanshawe College to start my journey to become an RRT. Although I didn’t know or realize it at the time, that weekend visit with my sister and her room-mate changed the course of my studies and set me on the path to the career I find myself honoured to be a part of today.
As mentioned I enrolled in the Respiratory Therapy program at Fanshawe College in 2003. Upon graduation in 2006 I started my clinical career at London Health Science Center Victoria Hospital (Vic). This was a great place to obtain employment right out of school. Working at Vic provided me with a number of opportunities to both challenge myself and engage in the profession. The staff at LHSC are like a giant family. Finding myself fortunate enough to become a member of the department was one of the highlights in my early career. I found myself working in the adult critical care unit, the trauma and emergency department, adult and pediatric wards and in the operating room. After the first summer working as an RRT, I picked up a second job working casually at Stratford General Hospital. Working in a smaller community hospital is vastly different then a major trauma hospital but just as rewarding. At Stratford I was fortunate enough to gain experience in some outpatient services, providing care and services to patients requiring cardiopulmonary diagnostics, ECG’s, Holters, Stress testing, Spirometry, PFT, etc. This is where I realized the breadth our career has to offer. Shortly after graduation, a faculty member (shout out to Sandy Annett) at Fanshawe College reached out and inquired if I would be interested in teaching part-time in the RT lab. This opportunity would change the course of my career once again and I haven’t looked back from trying to position myself to help and prepare the future of our profession.
Luckily, I have been surrounded by quality RT’s in my career that have modelled a number of attributes that I believe are a recipe for success. I suppose the proper answer to this question might be an RT who is a critical thinker and can troubleshoot problems, quickly and with accuracy, or the RT who is engaged in continuing professional development. Although I 100% agree with those things, I believe that this is what makes us a professional and required member of the healthcare team, this is what we train to do and with experience we can execute this with a high level of proficiency. However, the attribute that makes a “person” a quality RT in my opinion is someone who cares. That might sound obvious but I believe that each of us entered into this healthcare career because we truly care for the patients we interact with every day. Without the “care” part, our practice would come across cold and impersonal. A quality RT finds a way to connect with their patients and families, providing an individualized approach to what they do and how they do it. We all have our unique ways of doing this. I think patients expect us to have the knowledge, skill and abilities to perform, but when they realize that you are actually invested in their health and their well-being, that’s when I think something unique happens.
Preceptors play such a big role in a student’s progression. A good preceptor challenges and inspires a learner to want to be better. My approach is to acknowledge that learning is a two-way street and that I can learn just as much from the students as they hopefully can learn from me. I believe it comes down to communication. Often I find the preceptor may not want to give feedback for fear of upsetting a student, and maybe a student doesn’t want to ask their preceptor a question for fear of looking like someone who isn’t prepared. However, establishing a relationship that encourages open communication and constructive feedback is important for both parties involved and may break down the barriers that “fear” often promotes. I recall one of the more influential preceptors I had when I was a student sat me down at the beginning of the shift and simply just introduced themselves, she told me how long she was an RT for, what she loved about the job, what she found challenging and explained how she approached the assignment for the day. Without knowing it at the time, she broke down the barrier for me to think of her as someone who was evaluating me and judging me (even though she was), instead I felt comfortable enough to ask her questions and seek clarification when I was unsure. Simple but effective communication is often taken for granted.
As for students maximizing their clinical year, my hope is that they have prepared to the best of their abilities to take advantage of the opportunities that are presented to them. I appreciate that transitioning from a task trainer or simulation lab to the “real world” is nerve wracking but trust that you have a supporting team around you that has the patient’s best interest in mind and will guide you when able. I think Wayne Gretzky said it best “You miss 100% of the shots you don’t take” meaning you will never succeed if you don’t try.
I started working in the OR early on in my career at Vic. I volunteered to work in the OR because I wanted to get better skills at airway management. Working at Stratford General Hospital you were often the only RT on at night and if a trauma or code or elective intubation occurred the RT is often the primary airway manager. I used the experiences I gained in the OR at Vic to increase my confidence at being able to provide care for patients when I was the individual standing at the head of the bed. Ultimately, I found I liked the role in the OR, the technical aspect of the equipment was interesting, I liked helping out in A-cases (emergency cases) running rapid infusers or helping resuscitate. I liked assisting in the thoracic room with placing double lumen tubes, I liked placing arterial and venous catheters, assisting with epidurals and spinals and central lines. Learning about ultrasounds and transesophageal echos… There always seemed to be something new and exciting that kept me interested.
I was fortunate enough to be working in the OR at Vic when the first AA’s were trained and started practicing. I saw this as a progression from our established roles and enabled us to elevate what we do as well as demonstrate to the team what we are capable of doing. I was also fortunate enough to be working at the college with Dennis Hunter, a very influential person involved with bringing the Fanshawe program to life. Dennis was someone who saw the potential of the role and along with a number of individuals and the CSRT pushed to make it happen.
I’ve always thought of anesthesia as something between a science and an art form. When you witness an Anesthetist skillfully deliver and titrate a number of medications to achieve a steady state of anesthesia that is not too deep and not too lite and when finished, reverse everything in a timely fashion it is pretty amazing. At this point in my career I was fairly comfortable with ventilation, vascular access and airway management, however I knew that to become an AA I would need to improve on my understanding of drug delivery. With that the biggest area I had to improve upon was my pharmacology. I knew the common medications and the general indications but when you are holding the syringe, it changes, you’re responsible for dosing, additive effects, side effects, patients’ response, titrating to effect, etc, all of these things that I hadn’t really had to worry about before as an OR RT. I spent a lot of time learning from consultants and residents and other AA’s about techniques they use in specific situations and why. Everyone had a bit of a different take on how to provide an effective anesthetic and it was interesting to take all of that in. I still enjoy learning about pharmacology and anesthesia techniques, I even find myself listening to podcasts related to this topic (ACCRAC – Anesthesia and Critical Care Reviews and Commentary: is my suggestion for anyone interested in a good anesthesia podcast).
I would suggest to first get yourself into an OR to gain some experience. Investigate what type of surgeries your hospital is performing and talk with the Anesthetist to find out what their needs are. If there is an established role, see if you can shadow an AA for a day. There is a demand for AA’s across the country and I believe it will continue to evolve. It can be difficult to make the decision to go back to school after you have been out for a number of years. I was in the same boat. It was a conversation with a colleague and friend Paul Williams at the 2016 CSRT Conference in Ottawa that started the ball rolling for me. My situation was unique, our family was growing and I had an opportunity to take a parental leave from the college to be home with our daughter in 2017, my wife and I arranged our schedules so that every Friday I could be back on campus to attend classes to become an AA. My full time job since 2013 has been as an educator in the RT program at Fanshawe, it was strange to go from someone use to being at the front of the class giving the lecture to transitioning back to a student in the AA program. It was a great experience to be in a class with individuals from all over Southwestern Ontario who brought so many different experiences to the table. This experience has come full circle as this Fall I am teaching in the AA program along side Paul Williams here at Fanshawe. I’m excited and proud to be a part of both the RT and the AA programs.
I was fortunate enough to get into part-time teaching in the RT lab very soon after graduating from the program. As with most graduates I was eager to pay down some student debt and jumped at the opportunity to be a lab instructor. Honestly that’s where I thought it would end, I never really expected to make education my focus as a career. I happened to be in the lab one day when Sandy Annett who was the co-ordinator of the RT program at the time asked if I would like to fill in for another professor who would be off sick for the rest of the term. The course was Anatomy and Physiology which wasn’t something I studied in depth at University, I of course took the class as an RT student but the next thing I knew I was picking up a text book and getting ready for a lecture on the renal system. My first lecture was absolutely brutal, I essentially read from my powerpoint slides and completed a 2 hour lecture in about 30 minutes. I was dead on my feet at the front of the class. I went home after that lecture and knew that the students deserved better. I put everything into the next lecture and found it very rewarding to see the students engaged in the class. I got lucky with contracts as well, it seemed every semester after that there was another opportunity to pick up a course. Eventually I started to feel like if I wanted to be better and make a go of this as a career I needed to invest in myself. I enrolled in a Masters of Adult Education at Yorkville and eventually obtained a full-time Faculty position in the RT program at Fanshawe College. I don’t regret for a second the path my career has taken.
Typically the day will involve prepping for content delivery and either giving lectures or being in the lab or simulations. There is a lot of desk time that is used for email, office hours for students and program or faculty meetings.
Since COVID and the lock down, we have seen a big change in how we deliver theory courses. The majority of the RT program right now is delivered in an online format. It has been an adjustment for both the students and the faculty but as any good RT knows when there is a problem there is also a solution. Our students have been incredibly resilient and hit the ground running with the new learning formats. We are fortunate enough to have the ability to still deliver our practical experiences face to face. Our labs and simulations are still going which is a huge benefit for students to gain that experiential type of learning that I strongly believe is ideal for development and progression. Each day brings something new and even if it’s a course or lecture that you have taught in the past, there are always advancements and new practices, new research that constantly keeps us changing things to meet the standard of practice and the National Competency Framework.
One of my early roles in the RT program was to develop a high fidelity simulation course. We had been using simulation more and more in our program and wanted to structure something to ensure every student was getting equitable learning opportunities. A component of my masters research was to look at how simulation can be used to bridge the gap between in class and clinical learning. As a program we felt developing a course in our 4th semester would serve as a capstone to the in class and lab components of the program prior to the students going on to start their clinical practicum. With support from our division, I enrolled myself in the Simulation Instructor Training Course at the Center of Medical Simulation. I spent 1 week in Boston learning from some of the industry leaders like Jenny Rudolph and Walter Eppich. I feel it gave me the confidence to deliver a quality and well rounded experience to our students. With this I have greatly appreciated and been fortunate enough to learn from other RT leaders such as Karl Weiss and Gino DePinto who have been incredible from the onset with sharing and collaborating when it comes to simulation and education (Thanks guys!).
I love when you see the “ah ha” moments happen! When you help someone understand or connect the dots it’s a great feeling. Our students chose this program and profession and to be able to share in their learning is a great joy.
RT school is no cake walk. It takes determination, dedication and patience. I strongly suggest setting up and using a peer group to both lean on in the tough times and learn from. Learning is a social experience (even if it’s online), there is just as much incidental learning that occurs day to day than intentional learning and being open to every learning opportunity will set you up for success. You also have to remember to find time for you. Finding a balance between studying and life is incredibly important. The last thing that I would suggest is to realize that your professors and preceptors want you to succeed just as much as you do. Use their experiences and ask questions, be inquisitive, challenge yourself. Everyone learns in their own way, find what works for you and know that what you are learning isn’t just to get the right answer on a test but rather it is to help the patients you will take care of in the future.
Following the lockdown, we continued learning using an online delivery. This term we are again offering all of the theory courses online, while practical labs and simulations are still being offered face to face (with social distancing, universal masking, hand hygiene and increased emphasis on disinfecting and sanitizing equipment and high touch surfaces throughout the day). How we provide online learning varies, but we have made use of video conferencing software, demonstration video’s, online tutorials, drop in sessions, youtube (you can check out my youtube page Vent Jockey), we are committed to make it work and I’m confident our faculty team will!
I think gaining experience in as many avenues of the profession as possible helps. I felt that my early training at both a large teaching hospital mixed with a community hospital helped. I am not claiming to be an expert in everything our profession offers but by working in an outpatient clinic it helped when a student asked a question about Holters, or PFT’s for example. I think it is useful when you have done a few and can use your experiences to give advice or even resources to help.. The same goes for working in ICU and ER, wards, OR, labor and delivery, rapid response teams, home care, primary care, etc. Having those experiences gives you an ability to answer a question related to a specific avenue of practice. Along with that I think, the more things you try, the more you find out what you like and what you don’t. If being an instructor is something you are interested in, apply to your local college, see if they have the need for any teachers assistants or part time lab help or even picking up a course in a prep program like prehealth can lend insight into whether you like it or not. You may also find enjoyment in patient education and be interested in pursuing your CRE or CAE, etc. There are so many ways to be an educator in our profession, stay current, get involved with the profession and put yourself out there.
When the lock down occurred, we wanted to help as much as possible. Knowing that there was going to be a potential surge of ICU patients requiring mechanical ventilation, our program with the approval of the college mobilized our fleet of ventilators to be serviced and ready for patient use. It didn’t seem right to leave them locked up in a lab when there potentially could have been someone who could benefit from them. Along with that Yvonne Drasovean a colleague and friend asked if I would team up with her, her husband and his coworkers who are Toyota engineers to participate in Code Life Challenge. This was a challenge to design and produce a low cost, easy to use and easy to manufacture ventilator. It was an incredible experience to be a part of this multidisciplinary team, to show how working together a team could produce a ventilator in an unrealistic short period of time that actually worked. We lovingly named the ventilator the Covinator-FT (F for Fanshawe and T for Toyota) and arrangements are being made to have it transported to the RT lab at Fanshawe to hopefully inspire students to be innovative as well.

Lastly, I felt obligated to help out at the bedside. I previously stepped away from the bedside for a few years to focus on my educator role and my family life, but with this pandemic I almost felt guilty being at home knowing that I had some of the skills that could help these patients. I accepted a job at St.Thomas Elgin General Hospital and worked alongside an amazing staff that work tirelessly to provide the best patient care possible. I’m happy to continue to work casually at STEGH now while resuming teaching at Fanshawe this term.
Our program was fortunate enough to send 3 faculty and 13 students to Guatemala. It was a life changing experience for myself and all involved. We worked at four different clinics in rural Guatemala. The experience ranged from assisting with triaging, assessing patients respiratory status, vital signs, blood glucose, medication profiles, assisting with vaccinations, giving nebulized treatments, making educational material for the clinics and helping out in any way we possibly could. We stocked shelves in pharmacies, we mopped floors, we participated in physical therapy with some senior patients… whatever needed to be done we were there to try and help. There definitely was an initial shock by the conditions of some of the clinics and the lack of supplies, but the local staff made the best of what they had, didn’t complain and did what they could for their patients. It puts things into perspective when you realize what we take for granted in our healthcare system. I think we all came back from that experience viewing our work environments in a different light.

For anyone interested in volunteering abroad, I say do it! It definitely provided me with a heightened global awareness and it somehow makes you feel more connected. It’s humbling, challenging and rewarding and something I hope to be able to continue with.
The CSRT simulation network aims to provide a collaborative forum to foster and inform evidence informed simulation practice across Canada. It is a place where like minded people can come and gain access to subject matter experts right in our own profession. It is an impressive group of RT’s participating in this network. If you are someone who participates in simulation either from a learner standpoint or a developer, this may be a place you find interesting. COVID put a bit of a pause on our meetings as we all were quite busy, but we have hosted a number of journal clubs, there is a small but hopefully growing repository of scenarios and most importantly there is an opportunity to meet with peers and learn from each other.
I listen to and enjoy podcasts and find them to be a great way to learn something new. Greg and I have flirted with the idea of doing something like this for a while. We thought that there was a gap in podcast land where there are very few RT specific podcasts. We only have recorded a few shows but the format is to typically find a guest who has influenced the profession or has an interesting story or can inspire us or just simply is fun. The feedback from the listeners has been very positive so far even though it is an extremely low budget production (we actually don’t have a budget haha). We originally thought that it would just be the students who would listen to it, but soon we were getting comments from RT’s across the province. The host we use has analytic software that lets us see where people are tuning in from and some of the places have surprised us… we’ve had the Philippines, South Africa, a few in New York, it’s kind of a cool realization that a small pocket of people around the world are also looking for RT related podcasts…We are always looking for interesting episodes, so if there is anything you want to hear please let us know and we will see if we can put something together. Farzad, you are on our radar for a future episode!!!
I think this pandemic has shined a spotlight on what we can do as a profession. Every RT across the country stepped up and became leaders in their institutions. I think over the next few years we need to continue to position ourselves to have a strong voice in all things related to respiratory care. Moving forward I envision more and more advanced practices coming our way enabling us to work under medical directives. More than ever before RT’s are gaining interest and becoming involved with research and this can only lead to more leadership within our profession. Continuing education and professional advancement opportunities such as anesthesia assistant, advanced neonatal care, certifications such as the CRE, CAE, CTE keep coming our way. These are opportunities we need to take advantage of and continue to push ourselves for both our patients and our profession We make our own future.
Outside of work, we have a busy family life. I’m happily married with 3 kids (2 boys and 1 girl). I coach soccer and hockey and stay involved in a number of their activities. When we have some down time our favourite thing to do is unwind at the family cottage. Lately I’ve gotten into audiobooks as a way to relax (Talking to Strangers by Malcolm Gladwell is a must). In an attempt to stay active I still play hockey in a local beer league. We love to travel and explore, and hope once things settle down we can book our next trip.
I’ve never talked this much about myself and feel as though there isn’t much else to say haha.
Thank you, Dave, for sharing your insight and experiences! I am sure you a role model for many people.
To the readers of this post, thank you for reading all the way to the end. Please share with us your thoughts. If you enjoyed this post, please consider liking and sharing it with others who may benefit from it.
Here is a link to the LFPress with the ventilator loan: https://lfpress.com/news/local-news/coronavirus-fanshawe-college-hands-over-life-saving-medical-equipment-to-london-hospitals
If you like to check out Dave and Greg’s podcast,it can be found on Apple podcast, Spotify, anchorFM, likely some other carriers. https://anchor.fm/rtaudio
Happy RTing,
Farzad Refahi
October 5th, 2020
https://respiratory.blog/dave/