I first met Mr. Leonardo Faundez, at The Michener Institute, as he supervised one of our interprofessional courses. It was evident that he enjoyed his role as an educator. As a class, we learned about different programs, including ultrasound. His expertise in sonography is backed with an extensive work history including: sonographer at small healthcare facilities, clinical education specialist, entrepreneur, education consultant, adult education assessor, and ultrasound professor. He has performed these roles at various organizations including University Health Network, Aprende Canada (his company), Institute for Quality Management in Healthcare and Exact Imaging, and many others. It was no coincidence that he was first in my mind when I wondered about the role of ultrasound in respiratory care.
I have witnessed the utilization of ultrasound in different settings including, but not limited to, difficult radial art-line placement, FAST scans, and diagnosis of diaphragmatic paralysis and cardiac tamponade.
I had heard “Negative FAST” being yelled out which followed with a look of relief on everyone’s face; however, I never took the time to better understand the process.
Leonardo, I have heard the terms FAST and POCUS being thrown around. What can you tell me about them?
FAST stands for focused assessment with sonography for trauma. It is a type of ultrasound examination done in emergency situations when looking for pericardial effusion or hemoperitenum post trauma. It is mainly performed by emergency physicians, surgeons or paramedics. The idea is to look for free fluid (in this case blood) in spaces around the heart, liver, spleen and pelvis. Fresh blood appears anechoic (black) on ultrasound.
POCUS stands for point-of-care-ultrasound. I would say that FAST falls under POCUS in that the latter one also deals with rapid ultrasound examinations. However, POCUS may also include the ruling out of other pathologies such as abdominal aortic aneurysms, appendicitis, cholecystitis, among others. It is also mainly performed by physicians in different areas in the hospital.
What can you tell me about other uses of U/S in clinical setting?
Ultrasound is very useful when looking for pleural effusion, mark for thoracentesis, and assess diaphragm motion.
Besides looking specifically for pleural effusion, it may also be detected as an incidental finding when performing abdominal ultrasound. When assessing the liver and spleen, since these organs are adjacent to the diaphragm, it is easy to spot fluid present superior to the diaphragm, in the thoracic cavity. Since patients take the supine position when having an abdominal ultrasound, pleural fluid will follow gravity and so it will be visible posteriorly superior/above the diaphragm. When documenting the pleural effusion, it is important to state the amount (small, moderate or large), the laterality, and how they compare.
If a sonographer is involved with marking for thoracentesis, he/she will scan the patient and show the radiologist where the largest pockets of fluid are and the best way to get to them. The radiologist will then make the mark on the patient.
As per diaphragm motion, the M-mode (motion mode) may be used to graphically show the motion over time. The single line used by the M-mode is placed so that it crosses the diaphragm. The resulting display will show a wavy line representing the degree of diaphragmatic motion. The professional performing the ultrasound will need to collaboratively work with the respiratory therapist in the ICU in order to scan the patient with the ventilator on and off.
M-mode is also used, for instance, when measuring the fetal heart rate in utero as it displays motion of the palpating heart.
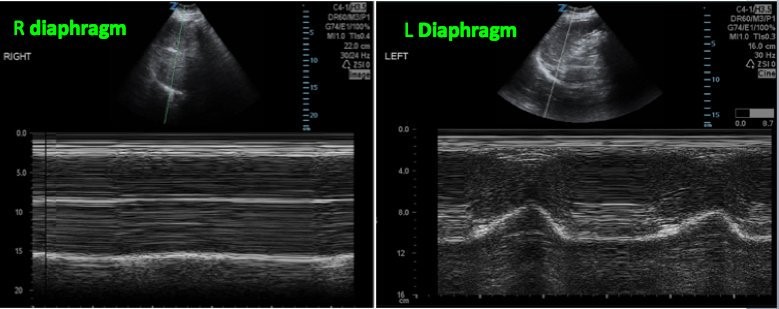
This image shows the M-Mode single line crossing the diaphragm (bright line shown by the arrow). The resultant graphical display shows a normal motion in the left diaphragm while no motion on the right side. https://twitter.com/sonostache/status/830999633371410432
Any other interesting overlap between respiratory system/care and U/S?
Ultrasound may also be used to assess for pneumothorax. Although ultrasound waves cannot travel through air, certain sonographic features allow the differentiation between normal air in the lung and pneumothorax. For more information on this, http://pie.med.utoronto.ca/POCUS/POCUS_content/lungUS.html
Thank you Leonardo for sharing your insight with me and others in the RT community!
To learn more about Leonardo and his work check out: www.aprendecanada.com .

Mr. Leonardo Faundez