I am excited to share with you my conversation with Thomas Piraino.

Tom needs no introduction but due to my diverse followers, I am going to share few words about him. Tom is a clinical specialist working at St. Michael’s Hospital in Toronto, Canada. His contributions expand to frequent talks at international conferences, and involvement with editorial boards such as Canadian Journal of Respiratory Therapy and American Association of Respiratory Care [1]. His published work ranges from original research to whole chapters in textbooks. He has received many awards from various organizations such as Canadian Society of Respiratory Therapists (CSRT), Respiratory Therapy Society of Ontario (RTSO), Hamilton Health Sciences, Fanshawe College, The Michener Institute and others [1]. I strongly recommend visiting the About Me portion of his website https://thomaspiraino.com/ for the full list of his contributions.
I first heard of Tom when we viewed one of his physiology and mechanical ventilation videos on YouTube in school. I began to recognize his name on many articles and publications. I have been lucky to attend few of his talks at different conferences, and it is no surprise that those conference rooms get filled within seconds and beyond capacity! When it comes to active RTs, he is one of my role models.
Let’s go back to the beginning of your career. When did you first hear about the respiratory therapy field? What made you consider respiratory therapy as a career?
Prior to becoming a Respiratory Therapist, I was a Medical Lab Technician working in a patient services lab taking blood and performing ECGs. I worked with a lady who really became like family to me. She encouraged me to look into Respiratory Therapy. She knew two Respiratory Therapists and thought I would be interested. She was right!
While you and your contributions are known to the RT community, I would like hear your perspective; What are some of your memorable jobs or roles so far?
I truly feel that all of my roles are memorable as they all helped me along my career path. The role I was in the longest was my educator role at St. Joseph’s Healthcare in Hamilton. I think my time and experience there helped me the most to advance professionally. I was able to work with an excellent group of RTs, and ICU physicians that were both supportive, inspiring, and motivated me to take a greater interest in research and how it effects best practice. My current job is like a dream job, I’ve been working in it for just over a year and it keeps getting more exciting.
As you continue to grow, expand and experience, have your career goals changed?
My career goals have evolved much like my career has evolved. What started out as a goal of obtaining a degree, has now evolved into a goal of obtaining a Masters. My personal life, other interests, and involvement in the profession outside of my day job has made this process slow, but I wouldn’t trade my experiences for anything else.
With various roles and responsibilities, what does a typical day look like for you?
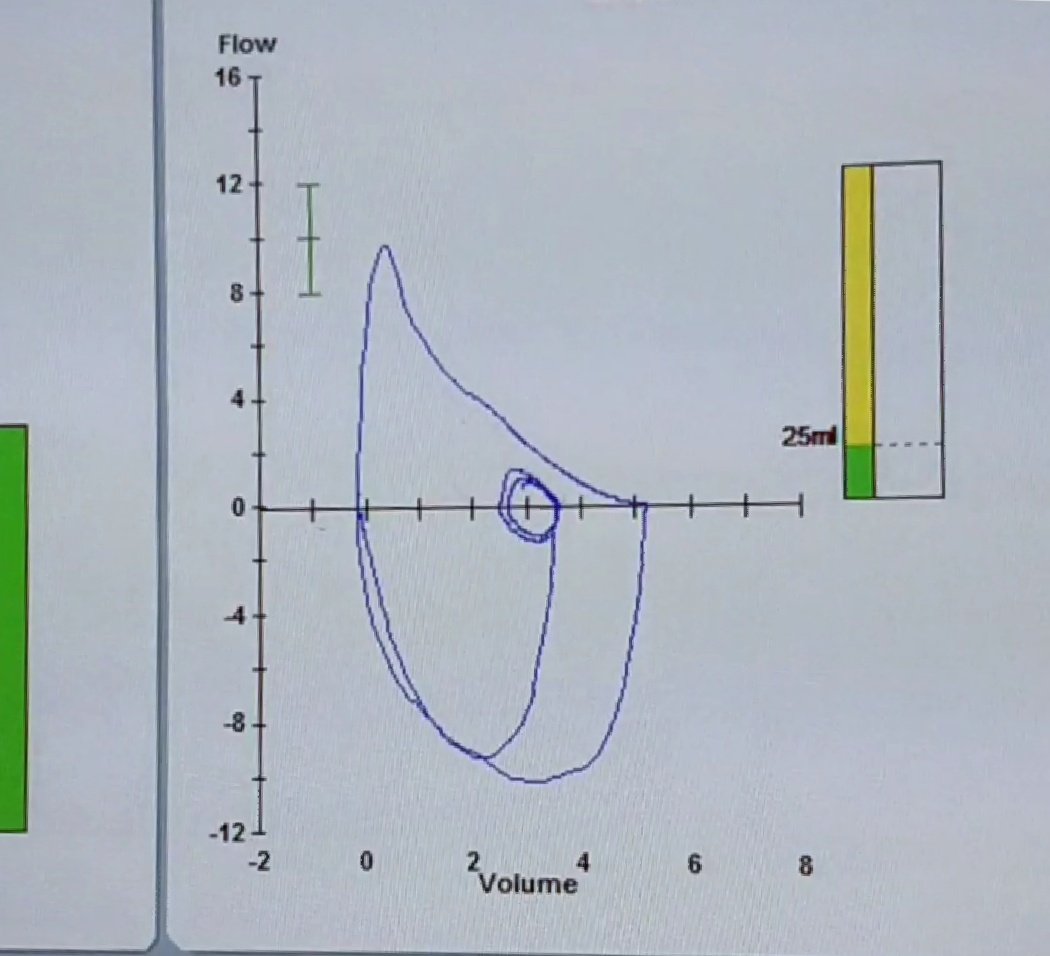
A typical day now involves spending time in the Intensive Care Unit at St. Michael’s both assessing patients for a number of research studies related to mechanical ventilation, and working with the bedside RTs and other members of the RT leadership team to translate research into bedside practice. Often this involves the use of technology such as electrical impedance tomography, esophageal balloon measurements, and ultrasonography. In fact, one of our big initiatives currently is to train the majority of our RT staff to perform diaphragm ultrasound measurements. It’s a very exciting time at St. Michael’s.
I will also spend time in the “lab”, which is a room in the hospital close to the ICU, where all of the international fellows currently working under Dr. Laurent Brochard spend their day. With the lab I help with a number of things related to research projects like developing study ideas and protocols, REB submissions, and working with industry partners to test and validate new equipment and software. I also help with performing bedside measurements for studies (ex. esophageal pressure measurements, diaphragm ultrasound). We have regular meetings related to our research projects, and hospital working groups dedicated to acute lung injury prevention. It is truly an inspiring place to work, and every day is exciting.
To reach higher levels require more than just hard work. What is your passion that drives you each day working as an RT?
When all the cool measurements and technology is stripped away, the underlying element that drives my passion is the patient and how vulnerable they are. The RT plays such a vital role in protecting the patient during the sickest time in the Intensive Care Unit because we are the ones responsible for setting up and manipulating the ventilator. For years now I have been speaking about the individualization of mechanical ventilation, and treating the individual patient using various measurements and monitoring, rather than treating every patient the same. It has been 8 years since I published editorials for the Lung Association (2010), and the RTSO (2011) regarding optimally setting PEEP, and using the term “individualized mechanical ventilation”, and at the 2013 CSRT conference my presentation was “Individualized Mechanical Ventilation for the ARDS Patient”. I’m happy to see now that this idea is being regularly mentioned in all the latest critical care articles (including the ATS guidelines for ARDS management published in May 2017) that care of the ventilated patient needs to be individualized.
You have been considered one of the top experts in pulmonary physiology, mechanical ventilation, and PEEP. How did you get involved with PEEP?
PEEP is the most elusive ventilator setting, and one that requires a much greater understanding of lung mechanics than we normally thinking about at the bedside. I have a strong interest in lung mechanics and bedside monitoring, so my involvement with PEEP and individualizing it came naturally.
What is your latest approach to PEEP?
My latest/favorite approach is using an esophageal balloon to determine the safety of the impact PEEP has on Plateau pressure and lung stress. And using EIT to balance distribution of ventilation in the lung, including overdistension and collapse.
Based on your observation, are bedside PEEP studies still done routinely?
PEEP studies are mostly done when other technologies are not available, but we should be cautious in blindly doing recruitment maneuvers and PEEP titration. A recent trial (ART Trial, published in JAMA) found higher mortality when using an open lung approach with recruitment maneuvers and decremental PEEP titration. There is a number of possible reasons for the results of this trial, but it clearly demonstrates that unrestricted use of recruitment maneuvers and high PEEP is still not the way to go, and is not as individualized as it seems when recruitability is not assessed beforehand.
Let’s step back and look at the RT field. Are you happy with the RT role?
I am happy with the RT role as I have taken part in it over the past 15 years, but I’m also not sure that the RT groups I have had the opportunity to work with represent the majority of the profession. I have been fortunate to work in hospitals that fully support innovative advancements to individualize the care we provide to patients. But there is much work to be done before this is a standard of practice in hospitals.
What is the next big growth area for the RT profession?
I think RTs should be more involved in research, and I think non-invasive monitoring tools to better understand the patient-ventilator interaction is also an area of potential growth with RTs. Again, I’m speaking about widespread adoption. Many RTs may be working in forward-thinking organizations that are doing new and innovative things, but again, it’s not the standard of practice.
In your opinion, what are qualities that makes a good/quality RT?
Be passionate, learn to understand and critique research, and speak up for your patient.
To prepare for this interview I consulted few RTs and this question came up few times: How does it feel to be an RT celebrity?
If people view me as an RT celebrity that is fine, but I’m really just an RT nerd. I’m VERY approachable, and love to meet people, so please don’t ever feel that you can’t come and talk to me, or message me on LinkedIn or Twitter.
To finish this interview I am going to ask a general question that is gaining more attention lately. What is your key to life-work balance?
My life-work balance is challenging, I’m not going to lie. I get involved in many things outside of my regular job, and I also have a part-time career as a web developer. I try my best to discipline myself to stay away from my phone and computer when my children are around, especially when doing an activity with them. However, once they are asleep, I begin to work on these other things, which means, I don’t sleep as much as I should. Additionally, I’ll work during my commute to work on the train.
Thank you Tom for taking the time to answer these questions. You are involved in so many projects and yet you took the time on your vacation to answer these questions. You are a source of inspiration for many RTs. Thank you for your contributions to our field!
To read more about Tom, view his blog and to contact him, check out his website at https://thomaspiraino.com/ . He is also on LinkedIn https://www.linkedin.com/in/thomaspiraino . If you use Twitter, you can also follow him @respresource.
References:
[1] Thomas Piraino. About Me. Accessed: May 16, 2018. https://thomaspiraino.com/about/
Image shared with permission of Thomas Piraino .
If you like to use the content of this blog, including the image, please ask for permission first.



 I first met Carolyn Greer at the 2017 CSRT conference in Halifax. After overhearing my name in a conversation, she approached me with a big smile and a determination to ask if I was the Farzad, ‘Raffi’, who will be joining Markham Stouffville Hospital’s PFT lab a few days after the conference. I have worked with Carolyn for the past 11 months in the PFT lab, and have been amazed by her level of drive, dedication, and care. She is proud to be an RT, and has worked in various areas including acute care, community care, home care and pulmonary function testing. She also has volunteered for CRTO and Lung Association. To recognize her dedication and to further understand her views and gain further insights, I asked her to answer few questions.
I first met Carolyn Greer at the 2017 CSRT conference in Halifax. After overhearing my name in a conversation, she approached me with a big smile and a determination to ask if I was the Farzad, ‘Raffi’, who will be joining Markham Stouffville Hospital’s PFT lab a few days after the conference. I have worked with Carolyn for the past 11 months in the PFT lab, and have been amazed by her level of drive, dedication, and care. She is proud to be an RT, and has worked in various areas including acute care, community care, home care and pulmonary function testing. She also has volunteered for CRTO and Lung Association. To recognize her dedication and to further understand her views and gain further insights, I asked her to answer few questions.